Treatment of Acne Vulgaris With a 650-microsecond, 1064nm Nd:YAG Laser: A Retrospective Study
Idowu D. Olugbade1, Anna C. Petty2, Joyce Imahiyerobo-Ip2
1The Warren Alpert Medical School of Brown University, Providence, Rhode Island, USA, 2Vibrant Dermatology, Dedham, Massachusetts, USA
Correspondence: Idowu D. Olugbade (idowu_olugbade@brown.edu)
Received: 24 October 2024 | Accepted: 19 November 2024
Funding: The authors received no specific funding for this work.
Keywords: Caucasian | pulse width | skin of color
Abstract
Background
The 650-ms, 1064-nm Nd:YAG laser device may provide superior efficacy and tolerability for the treatment of acne vulgaris over conventional treatments.
Aim
To evaluate the efficacy and tolerability of a 650-ms laser for the treatment of mild to severe facial acne vulgaris.
Patients/Methods
Records of 225 subjects with mild to severe facial acne vulgaris and treated with a 650-ms laser were reviewed.
Results
Subjects required a median of 3 treatments to achieve clearance. Clearance was achieved in 108/225 (48%) subjects. Adverse effects were limited to acne flare-ups and dryness. Treatment with isotretinoin was not required in 180/209 (80%) of subjects. A variety of topical and oral medications and non-laser procedures may be used in conjunction with the 650-ms laser without adverse effects. At the 6-month follow-up visit, the median Investigator Global Scale (IGA) score was 1.0 (almost clear). For most IGA-rated parameters differences between white patients and patients with skin of color were not statistically significant.
Conclusion
The 650-microsecond, 1064-nm Nd:YAG laser provides a safe and efficacious treatment of mild to severe acne in patients with white skin and skin of color.
Introduction
Acne vulgaris is a chronic inflammatory skin disorder that affects approximately 9.4% of the global population, [1]. The pathogenesis of acne involves dysseborrhea and hyperseborrhea, changes in the hyperkeratinization of the pilosebaceous duct, the presence of Cutibacterium acnes (C. acnes), inflammation, and hormones (including androgens, insulin, and insulin-like growth factor- 1) [2]. A variety of psychosocial and psychiatric comorbidities associated with acne have also been described[1, 3].
Recent guidelines for managing acne vulgaris [4] strongly recommend benzoyl peroxide, topical retinoids, topical antibiotics, and oral doxycycline. For severe acne or cases unresponsive to standard treatments, oral isotretinoin is advised. Combining topical therapies with different mechanisms, reducing reliance on systemic antibiotics, and incorporating intralesional corticosteroid injections when appropriate are effective strategies for effective acne management. For physical modalities, which include laser and light-based therapies, evidence is insufficient to develop guidelines.
Topical and oral agents often have a slow onset of action, side effects that can reduce patient compliance, limited efficacy for some individuals, and the risk of antibiotic resistance [5]. Additionally, isotretinoin's teratogenicity poses significant concerns [6]. Due to these challenges, energy-based devices have gained popularity for managing acne and its comorbidities. The effectiveness of these or any alternative treatments depends on their demonstrated efficacy, safety profile, and potential for high patient compliance.
The present study retrospectively evaluates the efficacy and tolerability of the 650-ms, 1064-nm Nd:YAG laser therapy for mild to severe facial acne vulgaris in 225 patients with white and skin of color.
Materials and Methods
Study Design
Electronic medical records of patients (n=225, aged 14–61 years) diagnosed with mild to severe facial acne vulgaris were reviewed. All patients had been treated with the 650-ms, 1064-nm Nd:YAG laser (Neo Elite, Aerolase Corp., Tarrytown, NY). The authors analyzed the number of treatments to achieve clearance as defined by the Investigator's Global Assessment (IGA) scale, adverse events, medications, and other non-laser procedures used in conjunction with the laser.
Acne Severity Determination
Acne severity was assessed at each visit using the IGA scale in which 0=clear skin, 1=almost clear, 2=mild, 3=moderate, and 4=severe, and 5=very severe. Patients were assigned an initial IGA score from the clinical photos taken immediately before the laser procedure. Each patient's IGA score was independently reviewed and unanimously between at least two investigators.
Procedure
Each patient's face was cleansed with a gentle cleanser and water and patted dry. Frontal, left, and right profile photographs of each patient were taken after each visit prior to laser treatment using an iPad (9.7 in., 2017/2018 Model, 5th/6th Generation. Apple Inc., Cupertino, CA). All procedures were performed without anesthetic or precooling. Patient eyes were protected using sealed eye shields and protective eyewear was worn by those in the treatment room.
Laser Treatments
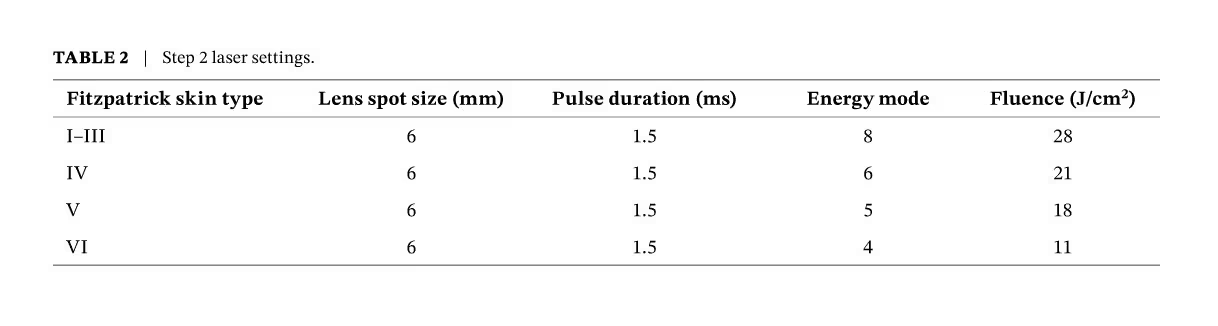
Laser settings were adjusted on the basis of Fitzpatrick skin type (Tables 1 and 2) to achieve the desired skin response to each laser pulse and to minimize the risk of burns, blisters, and erythema. Lower energies were used on patients with darker skin types. Laser treatments were performed in two steps (Tables 1 and 2). The treatment beam was applied to affected areas in a grid-like pattern with 6 passes using the 650-ms pulse width followed by 2 passes at 1500-ms pulse duration, thus addressing post-inflammatory erythema and stimulating collagen remodeling. Use of the longer pulse permitted treatment of post-inflammatory erythema and hyperpigmentation in all patients irrespective of skin color. Moisturizer and mineral-based sunscreen were applied immediately after laser treatment. Patients resumed their topical and oral medications, including topical retinoids.
In each treatment, the clinician monitored the heat sensation of the patient and adjusted the energy modes accordingly. For the most effective results; however, the clinician treated each subject with the highest energy mode possible for the skin type.
Table 1
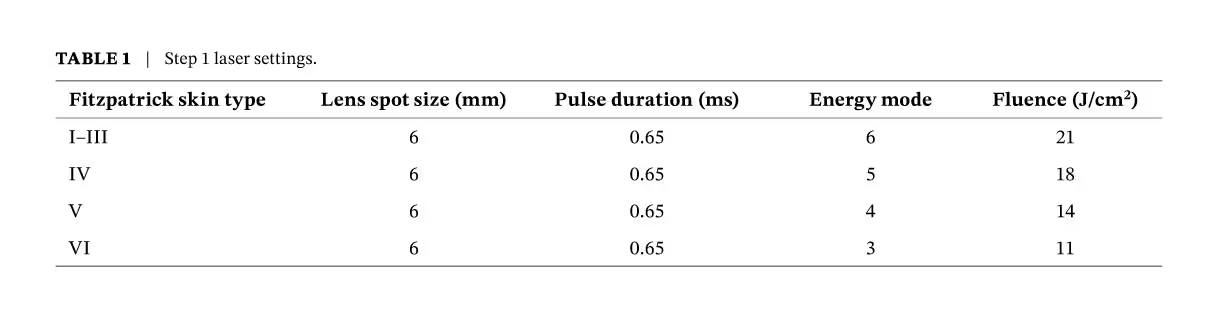
Table 2
Data Analysis
Subjects were categorized into two groups: white (Caucasian) and skin of color (African- American, Hispanic, Asian, and other races). The two groups were compared for the number of treatments to clearance, IGA scores at baseline and at 6 months, adverse effects, and the need for isotretinoin. The numbers for each parameter were small whole numbers with a short range, so a normal distribution of data was not assumed. Instead, a nonparametric Wilcoxon signed rank test was used for comparisons. In cases where the response was binary (yes or no), values of 1 and 0 denoted yes and no, respectively. Statistical analyses were conducted using Analyse-it Software, Leeds, U.K.
Results
Patient Demographics and Baseline Characteristics
A total of 255 patients completed one or more treatments. Among these, 89% self-identified as females and 11% as males. The majority of patients were Caucasian (41%) and African American (38%), while the remaining patients identified as Asian (9%), Hispanic (3%), and other (9%).
Number of Treatments and IGA Score
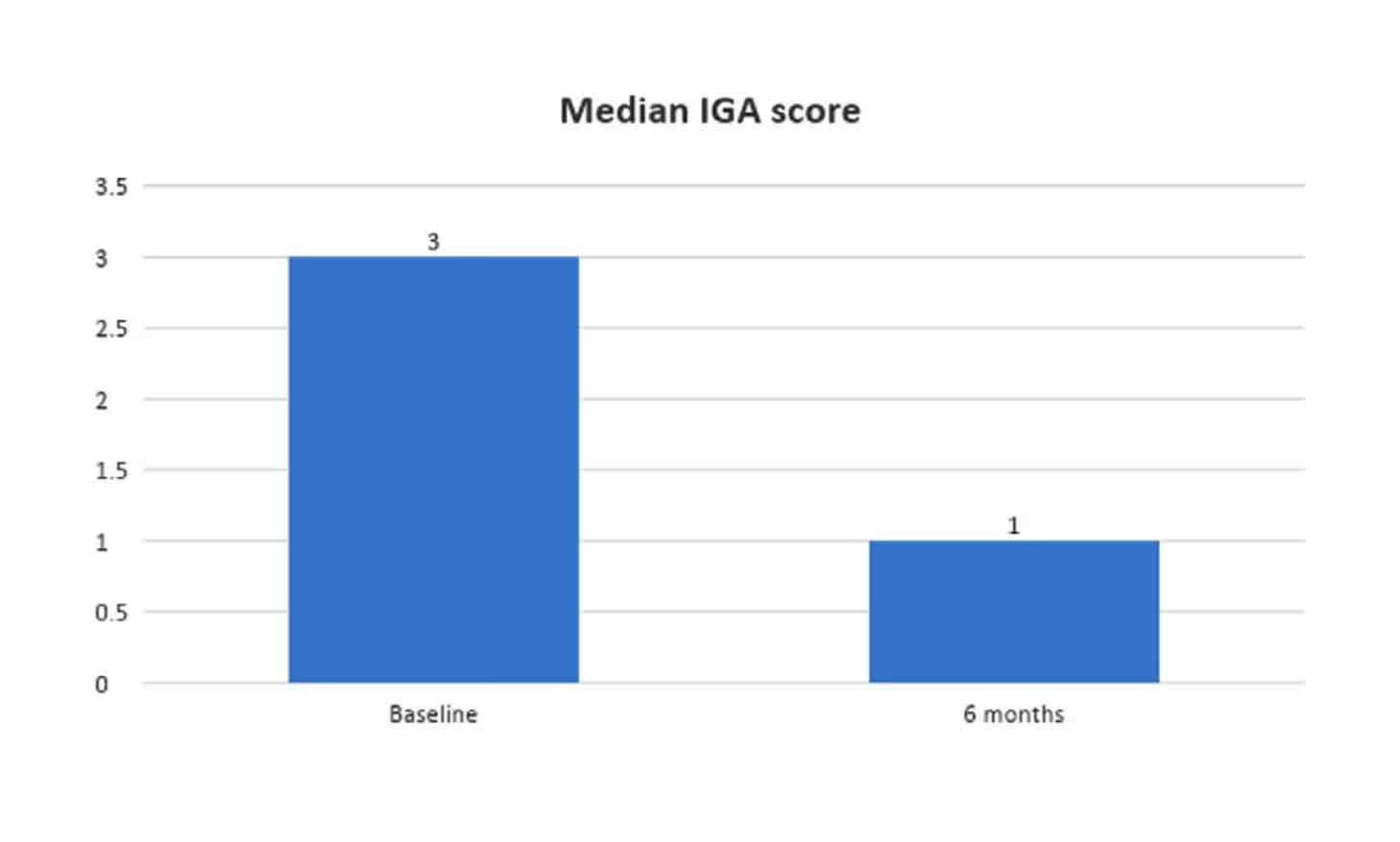
As shown in Figure 1, patients required a median of 3 treatments to achieve clearance. Clearance was achieved in 108/225 (48%) patients. Patients were evaluated 6 months after the laser procedure. Figure 2 shows the median IGA scores at baseline and at 6 months. The median score at baseline, 3, denoted moderate severity while the 6-month score was 1, or almost clear skin.
Figure 1
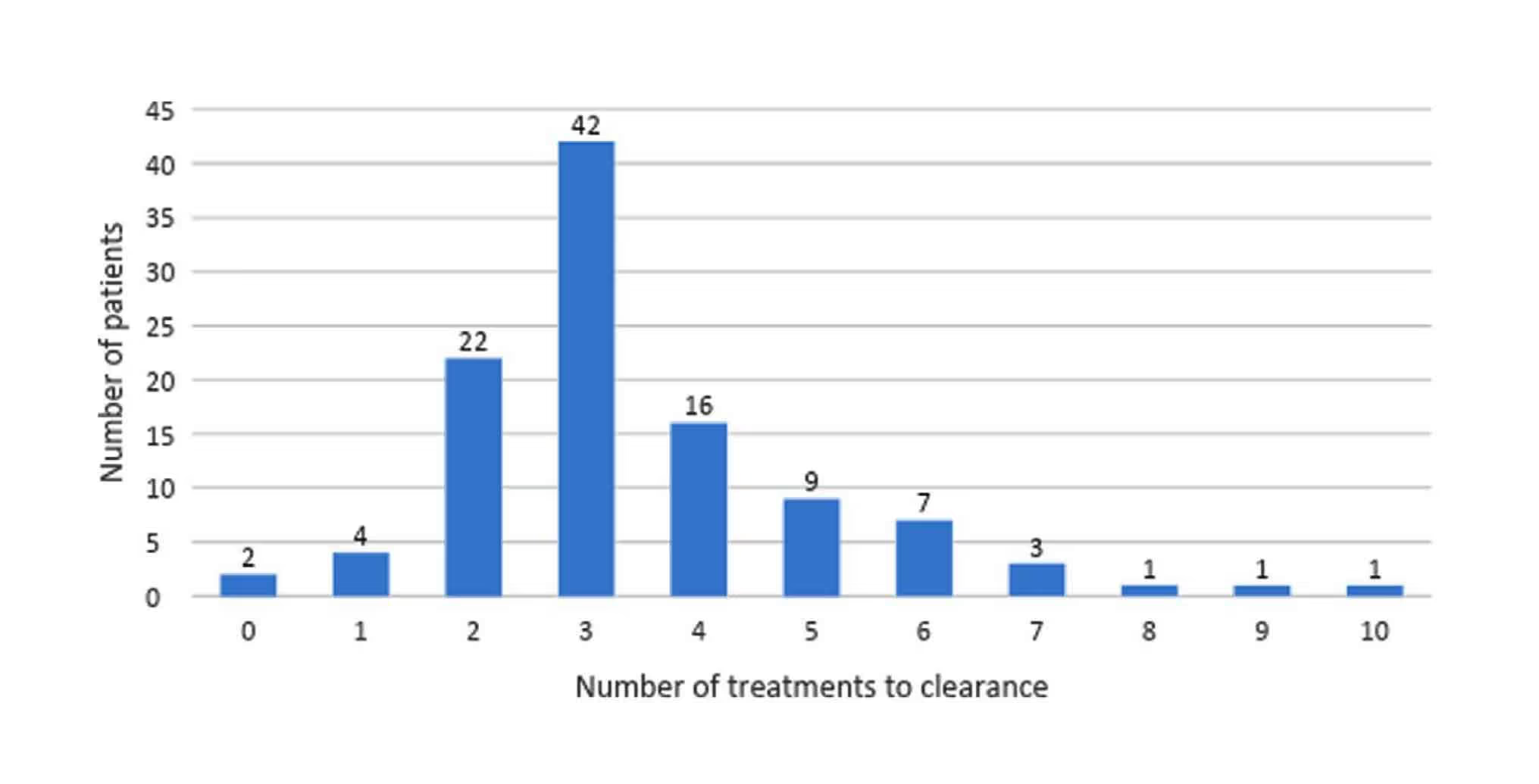
Figure 2
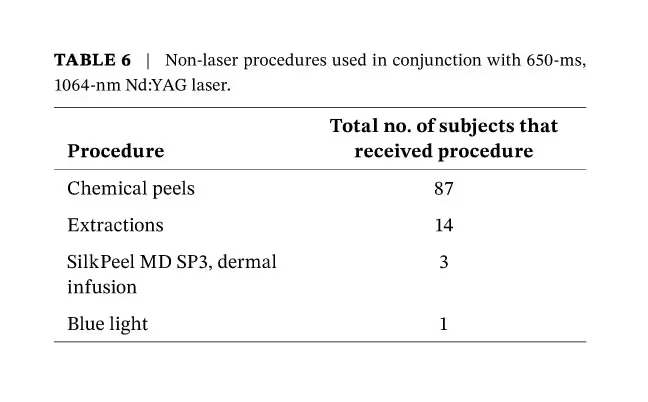
Adjunctive Therapies
Treatment with isotretinoin was not required in 180/209 (80%) of patients (Table 3). As shown in Table 4, a variety of topical medications were used in conjunction with the 650-microsecond laser. The most frequently employed were benzoyl peroxide (BPO), adapalene, azelaic acid, and minocycline. Oral medications are presented in Table 5, with 56.4% of patients requiring antibiotics and 17.3% requiring hormone-modulating therapies. When a patient achieved clearance, oral medications were discontinued. Additionally, some patients had a variety of non-laser procedures, primarily chemical peels and extractions (Table 6). The use of adjunctive therapies with the laser was well tolerated by patients and no adverse effects were observed.
Table 3
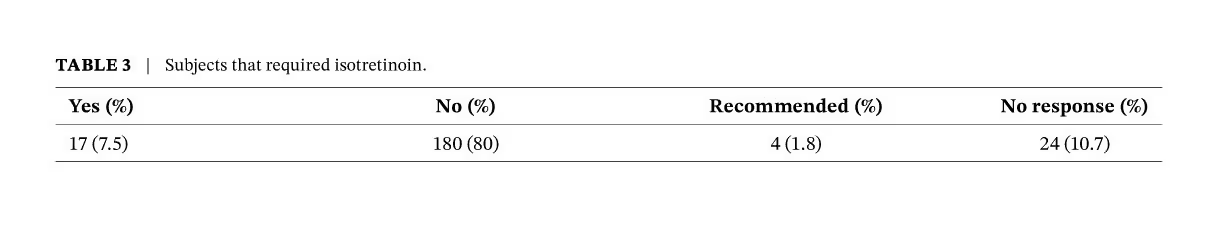
Table 4
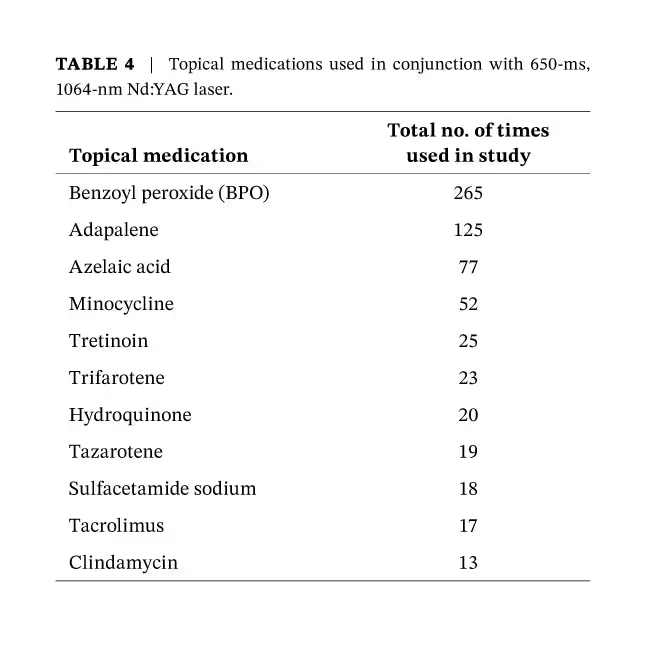
Table 5
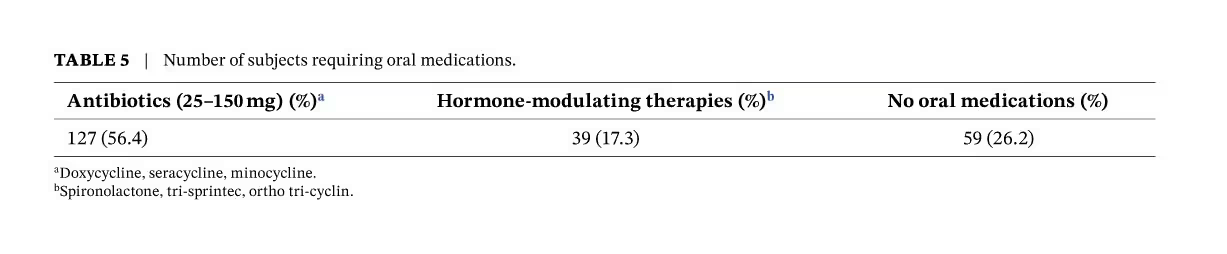
Table 6
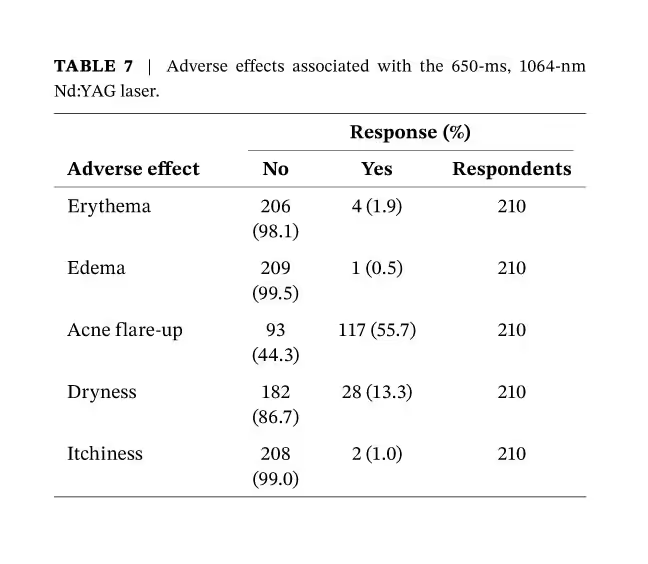
Adverse Events Assessment
Serious adverse events were not observed during the study. Non-serious adverse effects were recorded for 210 patients and broken down into 5 categories (Table 7). The most common adverse effects were acne flare-up (55.7%) and dryness (13.3%). The rest were limited to erythema (1.9%), edema (0.5%), and itchiness (1%).
Table 7
Treatment of White and Skin of Color Patients
As shown in Table 8, significant differences were not observed for the number of treatments to clearance, IGA scores at baseline and 6 months, need for isotretinoin, or adverse effects between white skin and skin of color. Clinical examples of patients treated with the 650-ms laser are shown in Figures 3–7.
Table 8
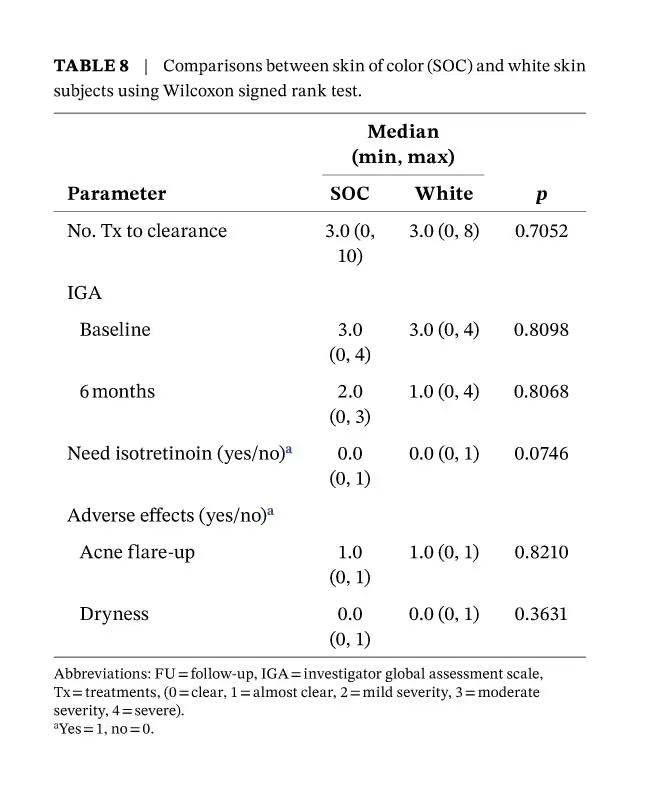
Figure 3

Figure 4

Figure 5

Figure 6

Figure 7

Discussion
The efficacies of energy-based devices for the treatment of acne have been reviewed [5, 7] and are summarized in Table 9. As the table shows, a variety of lasers have been used alone and in combination to treat acne. Blue light [10–12], red light [28], red and blue light in combination [8, 9] and intense pulsed light (IPL) [13, 14], for example, have all be used to treat acne. These devices target and damage key chromophores such as hemoglobin, melanin, porphyrins produced by C. acnes, and water. The photoactivation of these chromophores reduces sebum production and inflammation, destroys C. acnes, and increases collagen production [29].
Photodynamic Therapy (PDT), however, combines light energy with photosensitizing agent (aminolevulinic acid or methyl aminolevulinic acid), focusing on pilosebaceous units and C. acnes, thus taking advantage of the bacterium's production of photosensitizing porphyrins. This modality has considerable supporting evidence that includes 13 randomized clinical trials with 701 participants. PDT is typically used to treat patients with severe acne or acne that resists other treatments [30].
Light devices also have clinical disadvantages. Blue and red light, for example, are frequently combined due to their complementary antibacterial and anti-inflammatory properties, as well as deeper penetration of red light, resulting in a synergistic therapeutic effect [5, 31]. The disadvantage is that red and blue light therapy often requires multiple treatment sessions for optimal results [32]. PDT is limited by pain, erythema, and hyperpigmentation in patients with Fitzpatrick skin types III through VI [29, 33].
Canavan and colleagues [34] proposed that the efficacy of 400–1200 nm IPL might be due to its longer wavelengths because 1200 nm is an absorption peak of sebum. However, long-term follow-up data for IPL have not been reported and, for acne, this is important since C. acnes levels remain low only if light treatments are given over longer time periods, as with antibiotics [35]. Disadvantages of IPL include immediate erythema, burning, pain during treatment (with and without anesthesia), stinging, bulla formation, crusting, and hyperpigmentation [36].
Both the pulsed dye laser (PDL) and potassium titanyl phosphate (KTP) laser reduce levels of C. acnes by exciting light-sensitive porphryins [37]. Although patient numbers are small, and long-term treatment data are lacking for both modalities [15–17], the combination of PDL with PDT appears to be safe and effective for refractory inflammatory, comedonal, and cystic acne [38].
Mid-infrared lasers (1320, 1450, 1540 nm) are classified as lasers that destroy sebaceous glands because they target the depth of skin where the sebaceous glands reside. Each of these modalities require cooling to protect the epidermis[5]. For the 1320-nm laser, Deng and colleagues [17] reported six treatments to achieve the results in Table 9. Although a variety of studies have reported on the use of the 1450 nm laser[19–22, 24], treatment in one study[23] was accompanied by pain in areas with many inflammatory lesions and, with the 1540 Erbium glass laser, contact cooling was necessary during treatment [25]. Additionally, a randomized, split-face, investigator- blinded trial of facial acne[39] demonstrated that treatment with the 1450-nm laser did not reduce the inflammatory lesion count compared with the control.
Table 9
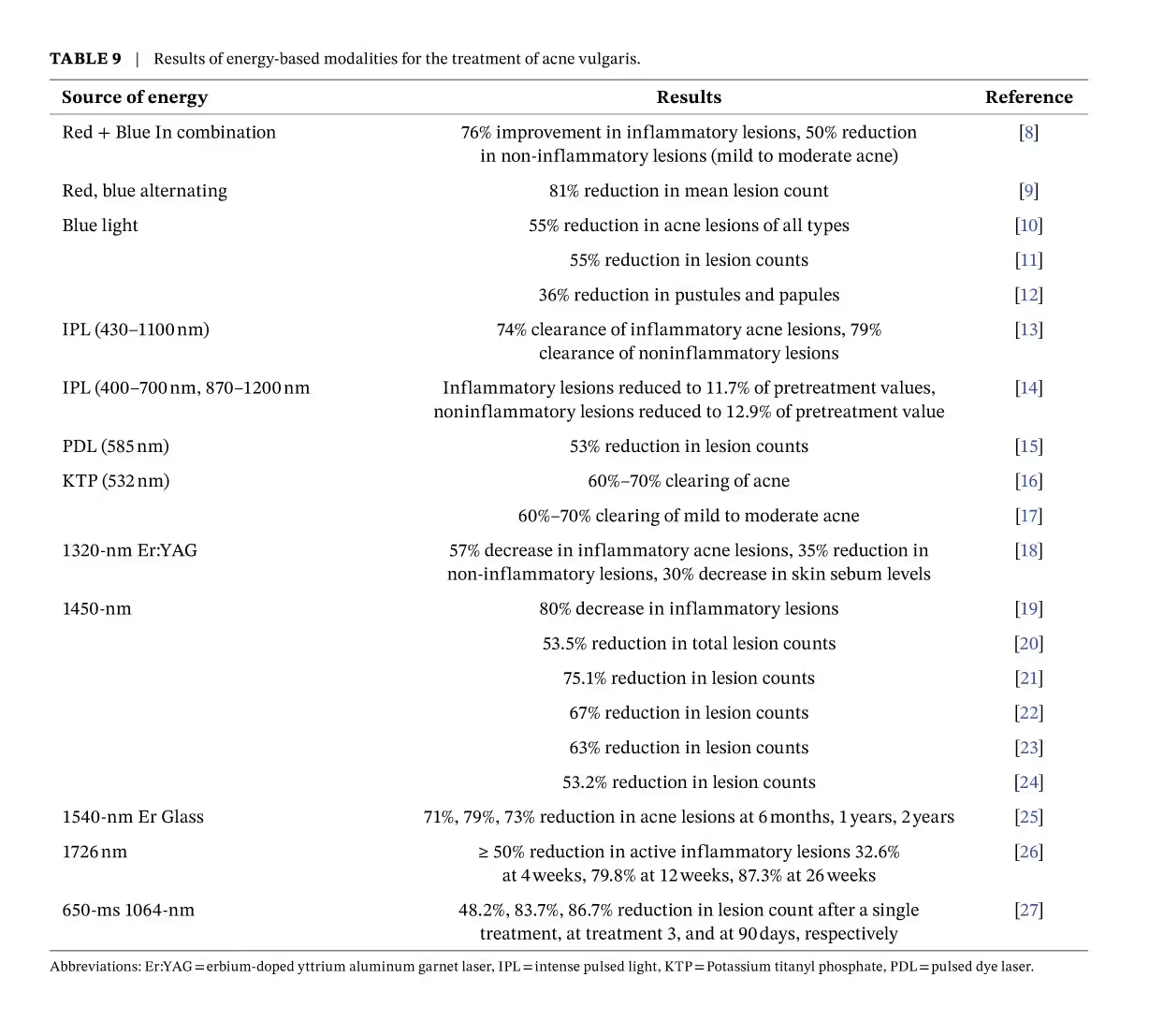
In their 104-patient study of patients with moderate to severe acne, Alexiades and colleagues[26] concluded that after three treatments, the 1726-nm laser was well tolerated and patients (Fitzpatrick skin types II–VI) showed progressive improvement over 26 weeks without serious adverse events.
Saedi and colleagues[27] showed that the 650-ms, 1064-nm laser, after 3 treatments, provided clearance for at least 90 days in patients with mild to severe acne. The treatments were well tolerated.
The 650-ms, 1064-nm Nd:YAG laser delivers high energy of short-pulse duration to target photoactive chromophores in the skin for the treatment of both acne and acne scarring. The laser also suppresses sebum production and reduces inflammation by inducing thermal coagulation of capillaries that supply sebaceous glands and inflamed skin lesions, resulting in shrinkage of sebaceous glands[5]. The 650-ms laser promotes collagenesis and remodeling by interacting with water for the reduction in acne scars and improvement in overall skin appearance[5, 33]. While previous studies have demonstrated the effectiveness of this laser in acne treatment, most have been limited to a small number of patients. To our knowledge, our study represents the largest retrospective analysis of the efficacy of the 650-ms, 1064-nm Nd:YAG in the treatment of mild to severe acne vulgaris and scarring in all skin types.
When treated with the 650-ms laser employed in this study, the majority of patients required only 2–4 treatments to achieve clearance of acne lesions. Notably, 48% achieved complete clearance. IGA scores were calculated for patients at each visit, showing a reduction from a median of 3 (moderate acne) at baseline to 1 (almost clear) 6 months post- treatment. This indicates that many subjects maintained clear skin months after completing laser therapy, demonstrating the sustained results of the treatment. It also shows that the 650-ms laser can be used in conjunction with various oral and topical medications, as well as non-laser procedures (e.g, chemical peels), without adverse events.
A major advantage of the 650-ms laser is its safety and efficacy in all skin types. This may be understood by considering the 650-ms pulse duration, which is shorter than the thermal relaxation time of skin tissue. This reduces the risk of pigmentary changes and scarring, making it a safe choice for skin of color[40, 41]. Statistical analysis of white and dark skin showed that the number of treatments to clearance, 6-month post-treatment IGA scores, need for isotretinoin, and adverse events did not differ significantly between the two groups, thus expanding treatment options for skin of color.
The overall results demonstrate the viability of the studied laser device as an alternative or adjunctive therapy for acne.
It shows effectiveness both with and without standard-of-care therapies, offering high tolerability and a favorable safety profile for all skin types. Considering these factors, high compliance is anticipated, addressing a key concern with many therapies.
Limitations of the present study include the absence of a control group and its retrospective design. The lack of insurance coverage for the present procedure may introduce selection bias because the study included only patients that could afford the procedure.
Conclusion
The 650-microsecond, 1064-nm Nd:YAG laser provides a safe and efficacious treatment of mild to severe acne in patients with white skin and skin of color.
Author Contributions
Joyce Imahiyerobo-Ip and Anna C. Petty were involved in the conceptualization and design of the study. Joyce Imahiyerobo-Ip and Anna C. Petty were responsible for study execution and completion. Anna C. Petty and Idowu D. Olugbade were responsible for data analysis. Joyce Imahiyerobo-Ip, Idowu D. Olugbade, and Anna C. Petty were involved in writing the original draft, reviewing, and editing. Joyce Imahiyerobo-Ip, Idowu D. Olugbade, and Anna C. Petty were involved in the final review and approval of the manuscript.
Ethics Statement
The collection and evaluation of all protected patient health information were performed in a HIPAA- compliant manner. General study informed consent and photo informed consent were obtained before performing study procedures and taking photographs. Permission for publication was also ascertained during the informed consent process.
Conflicts of Interest
Dr. Joyce Imahiyerobo-Ip is a consultant for Aerolase, and she has received no additional funding for the study or preparation of this manuscript.
Acknowledgments
We thank Morgan Shenaut, Julia L. Kane, and Elyse Korn for their assistance in collation of data, and Maya Dennis for providing writing assistance.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
1. J. K. Tan and K. Bhate, “A Global Perspective on the Epidemiology of Acne,” British Journal of Dermatology 172, no. Suppl 1 (2015): 3–12.
2. T. X. Cong, D. Hao, X. Wen, X. H. Li, G. He, and X. Jiang, “From Pathogenesis of Acne Vulgaris to Anti- Acne Agents,” Archives of Dermatological Research 311 (2019): 337–349.
3. P. Magin, J. Adams, G. Heading, et al., “Psychological Sequelae of Acne Vulgaris: Results of a Qualitative Study,” Canadian Family Physician 52, no. 8 (2006): 978–979.
4. R. V. Reynolds, H. Yeung, C. E. Cheng, et al., “Guidelines of Care for the Management of Acne Vulgaris,” Journal of the American Academy of Dermatology 90, no. 5 (2024): e1–e30.
5. M. H. Gold, D. J. Goldberg, and M. S. Nestor, “Current Treatments of Acne: Medications, Lights, Lasers, and a Novel 650-μs 1064-nm Nd:YAG Laser,” Journal of Cosmetic Dermatology 16 (2017): 303–318.
6. E. Bagatin and C. S. Costa, “The Use of Isotretinoin for Acne–An Update on Optimal Dosing, Surveillance, and Adverse Effects,” Expert Review of Clinical Pharmacology 13, no. 8 (2020): 885–897.
7. J. Bittar, P. Hooper, and J. S. Dover, “1726 Nm Lasers for the Treatment of Acne Vulgaris,” Skin Therapy Letter 29, no. 1 (2024): 5–7.
8. P. Papageorgiou, A. Katsambas, and A. Chu, “Phototherapy With Blue (415 nm) and Red (660 nm) Light in the Treatment of Acne Vulgaris,” British Journal of Dermatology 142 (2000): 973–978.
9. D. J. Goldberg and B. A. Russell, “Combination Blue (415 nm) and Red (633 nm) LED Phototherapy in the Treatment of Mild to Severe Acne Vulgaris,” Journal of Cosmetic and Laser Therapy 8 (2006): 71–75.
10. A. Kawada, Y. Aragane, H. Kameyama, Y. Sangen, and T. Tezuka, “Acne Phototherapy With a High-Intensity, Enhanced, Narrow-Band, Blue Light Source: An Open Study and In Vitro Investigation,” Journal of Dermatological Science 30 (2002): 129–135.
11. T. Y. Tzung, K. H. Wu, and M. L. Huang, “Blue Light Phototherap in the Treatment of Acne,” Photodermatology, Photoimmunology and Photomedicine 20 (2004): 266–269.
12. M. H. Gold, J. Rao, M. P. Goldman, et al., “A Multicenter Clinical Evaluation of the Treatment of Mild to Moderate Inflammatory Acne Vulgaris of the Face With Visible Blue Light in Comparison to Topical 1% Clindamycin Antibiotic Solution,” Journal of Drugs in Dermatology 4 (2005): 64–70.
13. M. Elman and G. Lask, “The Role of Pulsed Light and Heat Energy (LHE) in Acne Clearance,” Journal of Cosmetic and Laser Therapy 6 (2004): 91–95.
14. S. Kawana, R. Tachihara, T. Kato, and T. Omi, “Effect of Smooth Pulsed Light at 400 to 700 and 870 to 1,200 nm for Acne Vulgaris in Asian Skin,” Dermatologic Surgery 36 (2010): 52–57.
15. E. D. Seaton, A. Charakida, P. E. Mouser, I. Grace, R. M. Clement, and A. C. Chu, “Pulsed- Dye Laser Treatment for Inflammatory Acne Vulgaris: Randomised Controlled Trial,” Lancet 362, no. 9393 (2003): 1347–1352.
16. W. P. Bhaug and W. D. Kucaba, “Nonablative Phototherapy for Acne Vulgaris Using the KTP 532 Nm Laser,” Dermatologic Surgery 31 (2005): 1290–1296.
17. O. Yilmaz, N. Senturk, E. P. Yuksel, et al., “Evaluation of 532-nm KTP Laser Treatment Efficacy on Acne Vulgaris With Once and Twice Weekly Applications,” Journal of Cosmetic and Laser Therapy 13 (2011): 303–307.
18. H. Deng, D. F. Yuan, C. L. Yan, and X. A. Ding, “Fractional 1320 nm Nd:YAG Laser in the Treatment of Acne Vulgaris: A Pilot Study,” Photodermatology, Photoimmunology & Photomedicine 25 (2009): 278–279.
19. P. M. Friedman, M. H. Jih, A. Kimyai- Asadi, and L. H. Goldberg, “Treatment of Inflammatory Facial Acne Vulgaris With the 1450-nm Diode Laser: A Pilot Study,” Dermatologic Surgery 30, no. 2 Pt 1 (2004): 147–151.
20. S. Q. Wang, J. T. Counters, M. E. Flor, and B. D. Zelickson, “Treatment of Inflammatory Facial Acne With the 1,450 nm Diode Laser Alone Versus Microdermabrasion Plus the 1,450 nm Laser: A Randomized, Split- Face Trial,” Dermatologic Surgery 32 (2006): 249–255.
21. M. H. Jih, P. M. Friedman, L. H. Goldberg, M. Robles, A. S. Glaich, and A. Kimyai- Asadi, “The 1450- nm Diode Laser for Facial Inflammatory Acne Vulgaris: Dose- Response and 12- Month Follow- Up Study,” Journal of the American Academy of Dermatology 55 (2006): 80–87.
22. E. F. Bernstein, “A Pilot Investigation Comparing Low- Energy, Double Pass 1,450 nm Laser Treatment of Acne to Conventional Single-Pass, High- Energy Treatment,” Lasers in Surgery and Medicine 39 (2007): 193–198.
23. N. Konishi, H. Endo, N. Oiso, S. Kawara, and A. Kawada, “Acne Phototherapy With a 1450- nm Diode Laser: An Open Study,” Therapeutics and Clinical Risk Management 3 (2007): 205–209.
24. E. F. Bernstein, “Double- Pass, Low- Fluence Laser Treatment Using a Large Spot- Size 1,450 nm Laser Improves Acne,” Lasers in Surgery and Medicine 41 (2009): 116–121.
25. S. Angel, D. Boineau, S. Dahan, and S. Mordon, “Treatment of Active Acne With an Er: Glass (1.54 Microm) Laser: A 2- Year Follow-Up Study,” Journal of Cosmetic and Laser Therapy 8 (2006): 171–176.
26. M. Alexiades, A. Kothare, D. Goldberg, and J. S. Dover, “Novel 1726 nm Laser Demonstrates Durable Therapeutic Outcomes and Tolerability for Moderate- To- Severe Acne Across Skin Types,” Journal of the American Academy of Dermatology 89, no. 4 (2023): 703–710.
27. N. Saedi, T. Griffin, and S. Kelly, “Treatment of Mild to Severe Acne Vulgaris With a 650-Microsecond 1064- nm Laser.”
28. Y. Wu, Y. Deng, and P. Huang, “Application of Red Light Therapy for Moderate- To- Severe Acne Vulgaris: A Systematic Review and Meta-Analysis,” Journal of Cosmetic Dermatology 20, no. 11 (2021): 3498–3508.
29. C. Fenton and C. Kang, “Limit Acne Damage With Lasers and Light Therapy,” Drugs & Therapy Perspectives 39 (2023): 20–25.
30. H. J. Kim and Y. H. Kim, “Exploring Acne Treatments: From Pathophysiological Mechanisms to Emerging Therapies,” International Journal of Molecular Sciences 25, no. 10 (2024): 5302.
31. M. K. Li, C. Liu, and J. T. S. Hsu, “The Use of Lasers and Light Devices in Acne Management: An Update,” American Journal of Clinical Dermatology 22, no. 6 (2021): 785–800.
32. E. Nakayama, T. Kushibiki, Y. Mayumi, et al., “Optimal Blue Light Irradiation Conditions for the Treatment of Acne Vulgaris in a Mouse Model,” Journal of Photochemistry and Photobiology. B 239 (2023): 112651.
33. M. Boen, J. Brownell, P. Patel, and M. M. Tsoukas, “The Role of Photodynamic Therapy in Acne: An Evidence-Based Review,” American Journal of Clinical Dermatology 18, no. 3 (2017): 311–321.
34. T. N. Canavan, E. Chen, and B. E. Elewski, “Optimizing Non-Antibiotic Treatments for Patients With Acne: A Review,” Dermatol Therory 6 (2016): 555–578.
35. P. Babilas, S. Schreml, R. M. Szeimies, and M. Landthaler, “Intense Pulsed Light (IPL): A Review,” Lasers in Surgery and Medicine 42 (2010): 93–104.
36. E. J. Lee, H. K. Lim, M. K. Shin, D. H. Suh, S. J. Lee, and N. I. Kim, “An Open- Label, Split- Face Trial Evaluating Efficacy and Safety of Photopneumatic Therapy for the Treatment of Acne,” Annals of Dermatology 24 (2012): 280–286. 9 of 10 14732165, 0, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jocd.16711 by Test, Wiley Online Library on [13/01/2025]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
37. D. Thiboutot, H. Gollnick, V. Bettoli, et al., “Global Alliance to Improve Outcomes in Acne. New Insights Into the Management of Acne: An Update From the Global Alliance to Improve Outcomes in Acne Group,” Journal of the American Academy of Dermatology 60, no. 5Suppl (2009): S1–S50.
38. M. Alexiades- Armenakas, “Long- Pulsed Dye Laser- Mediated Photodynamic Therapy Combined With Topical Therapy for Mild to Severe Comedonal, Inflammatory, or Cystic Acne,” Journal of Drugs in Dermatology 5, no. 1 (2006): 45–55.
39. S. Darné, E. L. Hiscutt, and D. C. Seukeran, “Evaluation of the Clinical Efficacy of the 1,450 nm Laser in Acne Vulgaris: A Randomized Split- Face, Investigator- Blinded Clinical Trial,” British Journal of Dermatology 165 (2011): 1256–1262.
40. M. H. Gold, N. E. Manturova, L. S. Kruglova, and E. V. Ikonnikova, “Treatment of Moderate to Severe Acne and Scars With a 650- Microsecond 1064- nm Laser and Isotretinoin,” Journal of Drugs in Dermatology 19, no. 6 (2020): 646–651.
41. C. Burgess, S. Chilukuri, D. A. Campbell- Chambers, M. Henry, N. Saedi, and W. E. Roberts, “Practical Applications for Medical and Aesthetic Treatment of Skin of Color With a New 650- Microsecond Laser,” Journal of Drugs in Dermatology 18, no. 4 (2019): s138–s143.