The Use of Neodymium Laser in the Treatment of Vulval Dystrophies
Y.E. Dobrokhotova1, A.Y. Azimova1, E.I. Borovkova1, I.Y. Ilyina1, D.M. Ibragimova1, I.I. Grishin1, E.S. Platova2, V.I. Komagorov1
1Pirogov Russian National Research Medical University, Moscow, Russian Federation
2N.I. Pirogov City Clinical Hospital No. 1, Moscow, Russian Federation
Abstract
Aim: to assess effectiveness of the Aerolase Neo neodymium laser with a 1064 nm wavelength and 650 ms pulse duration in the treatment of patients with chronic vulvar dystrophies.
Patients and Methods: the study included 60 patients with lichen sclerosus and vulvar leukoplakia. Patients with the verified diagnosis of early-stage vulvar lichen sclerosus were randomly assigned to 2 groups. Group 1 consisted of 45 patients who were treated with the Aerolase Neo laser and group 2 consisted of 15 patients who applied topical clobetasol propionate 0.05% ointment over the vulvar area for 2 months: two times per day before the symptoms relieved and then — once per day, depending on the intensity of clinical manifestations, for 6 months. A comprehensive medical exam of patients was performed before and after treatment.
Results: histological examination revealed that the group 1 patients had a brighter red staining of the stromal collagen fibers demonstrating a pronounced collagenization of the stroma after the treatment. In the group 2 patients the examination results did not demonstrate any significant changes. The number of complaints associated with vulvar dystrophies significantly decreased among the group 1 patients who received laser therapy, and they also reported a higher satisfaction with the quality of sexual life. Those patients who used topical glucocorticoids noted there cured itching in the vulvar area which required the continuation of maintenance therapy for up to 6 months and suggested that glucocorticoids provided a short-term effect.
Conclusion: the obtained results prove the effectiveness of neodymium laser therapy for patients with vulvar dystrophies thus providing a rationale for using this method of treatment.
KEYWORDS: lichen, leukoplakia, chronic vulvar dystrophies, neodymium laser, laser therapy, sexual life.
FOR CITATION: Dobrokhotova Yu.E., Azimova A.Yu., Borovkova E.I. et al. The Use of Neodymium Laser in the Treatment of Vulval Dystrophies. Russian Journal of Woman and Child Health. 2023;6(*):1–8 (in Russ.). DOI: 10.32364/2618-8430-2023-6-*-1-8.
Introduction
Chronic dystrophic diseases of the vulva (CDV) are diagnosed in all age groups, from childhood to postmenopausal age. At the moment, they are the least studied diseases of the female reproductive system. The vulva consists of the labia minora, labia majora, pubis, and the vestibule of the vagina. At the frontal part of vulvar vestibule are the outer surface of the hymen and the frenulum of the clitoris. At the posterior part is the posterior commissure and on the sides is the Hart's line, which is the line of transition of non-keratinizing squamous epithelium to keratinizing epithelium of the vulva. [1]. Chronic dystrophic (non-inflammatory) diseases of the vulva and perineum are pathological changes characterized by damage to the external genital organs and the mucous membrane of female internal genital organs1. In clinical practice, CVD goes by the following names: kraurosis, lichen sclerosus, sclerotic dermatitis, lichen sclerosus, atrophic vulvitis, senileatrophy, vulvar leukoplakia [2].
In 1993, the International Society for the Study of Vulvovaginal Disease and the International Society of Gynecological Pathologists adopted the following classification of diseases of the vulva, which is currently widely used throughout the world and is based equally on clinical and histological signs [2].
I. Benign lesions of the vulva:
- Lichen sclerosus
- Squamous hyperplasia
- Other dermatoses
II. Vulvar intraepithelial neoplasia:
- mild
- moderate
- severe
Dystrophic diseases develop sequentially and are characterized by the appearance of itchy white spots. Scratching then causes chronic trauma to the vulva accompanied by an inflammatory response and tissue scarring. Leukoplakia of the vulva and sclerotic lichen can be recognized by constant itching in the intimate place, which increases with urination and movement. Dystrophic diseases drastically reduce a woman's life quality, leading to exhaustion of the nervous system up to the loss of working capacity.
Symptoms of lichen sclerosus include:
- itching in the vulva, especially at night
- burning in the vulva
- pain during intercourse (dyspareunia)
- pain in the vulva (vulvodynia)
- dryness and tightness of the external genital organs
- progression of wrinkling and sclerosus of the vulva
- pain during bowel movements and urination
Currently, there is no classification according to the severity of lichen sclerosus. However, in 2018, a classification where the disease was divided into early and late stages was adopted [3].According to this classification, in the early stages, patients complain of mild discomfort in the vulva, most often represented by mild itching or burning. In more advanced stages, in addition to the symptoms described above, cracks and erosion appear in the vulva area, progression of atrophic processes, and the formation of synechia (unions) of the labia minora and labia majora are observed. Subjective symptoms associated with neuro sensory disorders, such as itching, burning, and pain on touch, are more pronounced and are present both at rest and when moving.
In turn, vulvar leukoplakia, or squamous cell hyperplasia, is practically asymptomatic, and only when the symptoms are pronounced, patients complain of burning or itching.
In recent years, there has been an increase in the number of patients with dystrophic diseases of the vulva and, subsequently, an increased incidence of vulvar cancer, which allows us to consider this problem relevant from the stand point of not only timely diagnosis but also prevention of vulvar cancer [2].
Leukoplakia is often found in comorbidity with vulvar lichen sclerosus but can also be an independent disease. At the same time, malignant cells of the vulva are exposed mainly to foci of leukoplakia and not to foci of sclerosing lichen. Thus, as indicated in the work of L.E. Sharapova[2], dysplasia and preinvasive cancer are revealed histologically more often in leukoplakic plaques rising above the skin surface than in flat white spots.
Steroid hormones affect the tissues of the vulva by interacting with specific receptors. Therefore, a decrease in estrogen plays a significant role in the occurrence of dystrophic processes in the vulva.
The pathogenesis of dystrophic processes in the vulva affects all parts of the neuroendocrine system. L.A. Ashrafyanet al. [4] noted a high incidence of diseases in patients with CVD due to impaired fat, carbohydrate, and other types of metabolic components. At the same time, many authors have identified the relationship between these diseases of the vulva and several autoimmune pathologies, such as auto immune thyroiditis, systemic lupus erythematosus, etcetera [5].
The pathogenesis of squamous cell hyperplasia of the vulva is characterized by an inadequate proliferative response of the epithelium. Three components are involved in the pathogenesis of vulvar sclerosing lichen (LVS): onset of autoimmune mechanisms, disruption of fibroblast and collagen homeostasis, and inflammation, which in turn induces oxidative stress.
The most common symptoms of these diseases are itching and burning in the vulva. Together with dyspareunia, they have a significant impact on the life quality and sexual health of women.
To date, the treatment of chronic dystrophic diseases of the vulva is a long-term use of local potent glucocortico steroids.
Ointments for external use are also used: weak corticosteroid - triamcinolone 0.1%, moderate cortico steroid-betamethasone 0.1%, strong corticosteroid - clobetasol 0.05%[1].
The most widely used and recommended as the "gold standard" treatment for vulvar lichen sclerosus (LSV) is the topical application of ultra potent corticosteroid ointments, especially 0.05% clobetasol propionate ointment [6, 7]. The anti-inflammatory properties of clobetasol help reduce inflammation and obstruct the progression of the disease.
However, it should be noted that many patients refuse to take hormonal drugs, or there are contraindications to their use. Due to low compliance and the possibility of experiencing adverse effects, alternative therapies are also welcome.According to the literature, it is possible to use lasers for the treatment of chronic dystrophic diseases of the vulva [8].
The purpose of the study is to study the effectiveness of the Aerolase Neo neodymium laser with a wavelength of 1064nm and a pulse duration of 650 ms in the treatment of patients with CVD.
Materials and Methods
The Department of Obstetrics and Gynecology of the Medical Faculty of Pirogov Russian National Research Medical University of the Ministry of Health of Russian Federation and the Department of Gynecology of the N.I. Pirogov City Clinical Hospital No. 1 conducted a randomized study in parallel groups, which involved 60 patients with a morphologically confirmed diagnosis of vulvar squamous cell hyperplasia and lichen sclerosus at an early stage. The study was approved by the local ethics committee of Pirogov Russian National Research Medical University. All patients signed an informed voluntary consent to participate in the clinical study.
The criteria for inclusion of patients in the study were histological confirmation of the diagnosis, the absence of severe comorbidities, and a written consent to treatment. The clinical diagnosis was established on the basis of patients' complaints, anamnesis, and the results of a morphological histological examination of pathologically altered vulvar tissues. All collected histological material was available for research.
Patients with a confirmed diagnosis of early stage vulvar lichen sclerosus (LSV) were randomized into two groups. Group 1 included 45 patients who underwent exposure to Aerolase Neo neodymium laser. Group 2 included 15 patients who applied glucocorticoids (GCs) locally to the vulva area.
As for the protocol for the neodymium laser, the procedure did not require anesthesia. However, in some cases, due to the high sensitivity of the clitoral zone, local anesthesia with anointment containing lidocaine and prolacaine was used 15–20minutes before the session. A focal lens F was used: spot diameter 2 mm (red lens with holders) in Energy Mode 4.5–5.0 (1.5–2.0 Hz). The area of irradiation necessarily included a portion of normal tissue, 3–5 mm from the edges of the affected area. The area of the urethra, vulva, and perianal area fell under the effect of irradiation. Several complete passes were carried out, from 3 to 5, depending on the disease severity and pain sensation. To obtain a visible result, as a rule, several sessions were required. The treatment effectiveness also depended on the severity, depth, and size of the lesion. The treatment protocol included from eight to 10 procedures completed within 2–3 weeks.
In Group 2, patients used 0.05% clobetasol propionate ointment for two months, two times a day until the symptoms subside, then once a day at night, then every other day at night for 6 months, depending on the intensity of clinical manifestations.
Before treatment, the patients underwent a vulvar biopsy with a round scalpel "Dermopanch" with a diameter of 4 mm.After completion of treatment, a vulvar biopsy was performed again for a comparative analysis of histological materials. The materials obtained through the second vulvar biopsy after the treatment were collected from the same site as before the treatment. The histological material of the vulvar biopsy was fixed with neutral (buffered pH 7.0) 10–12% formalin. In histological sections, pathoanatomical features were also evaluated in both study groups. For the coloring of the material, Van Gieson's stain was used.
The objectification of complaints and control of the effectiveness of the treatment was carried out by evaluating the validated questionnaire PISQ-12 (Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire), recommended for use in clinical practice by the International Urogynecological Association and allowing a qualitative assessment of three areas: behavioral-emotional, physiological, and sexual. The sum of points was calculated, and based on the sum, the answers of the patients from the studied groups to the questions of the PISQ-12 questionnaire were evaluated. The survey results were interpreted as follows: from 0 to 10 points - worsening, from 11 to 20 points - no change, from 21 to 30 points - improvement in sexual function. We studied the dynamics of the severity of LSV symptoms, assessed using a 10-point visual analog scale (VAS), where 0 points is no symptom, and 10 points is the highest symptom severity. The study also assessed the side effects of the treatment.
Standard statistical methods were used to process the results of the study.
Study Results
A comparative analysis of clinical and anamnestic data between the groups revealed no statistical differences. The average age of patients in both groups was 53, ±2.5 years. When collecting anamnesis, it turned out that the average age of menopause was 50.4, ±2 years. When analyzing comorbidities in patients with chronic dystrophic diseases of the vulva, the predominance of chronic autoimmune thyroid diseases was revealed in 14 (23.3%) patients, which confirms the literature data that endocrine and autoimmune diseases are the most common among patients with LSV [5].
Histological examination revealed 52 (86.7%) out of 60 patients had LSV only, and 8 (13.3%) out of 60 patients had LSV in combination with squamous cell hyperplasia of the vulva.
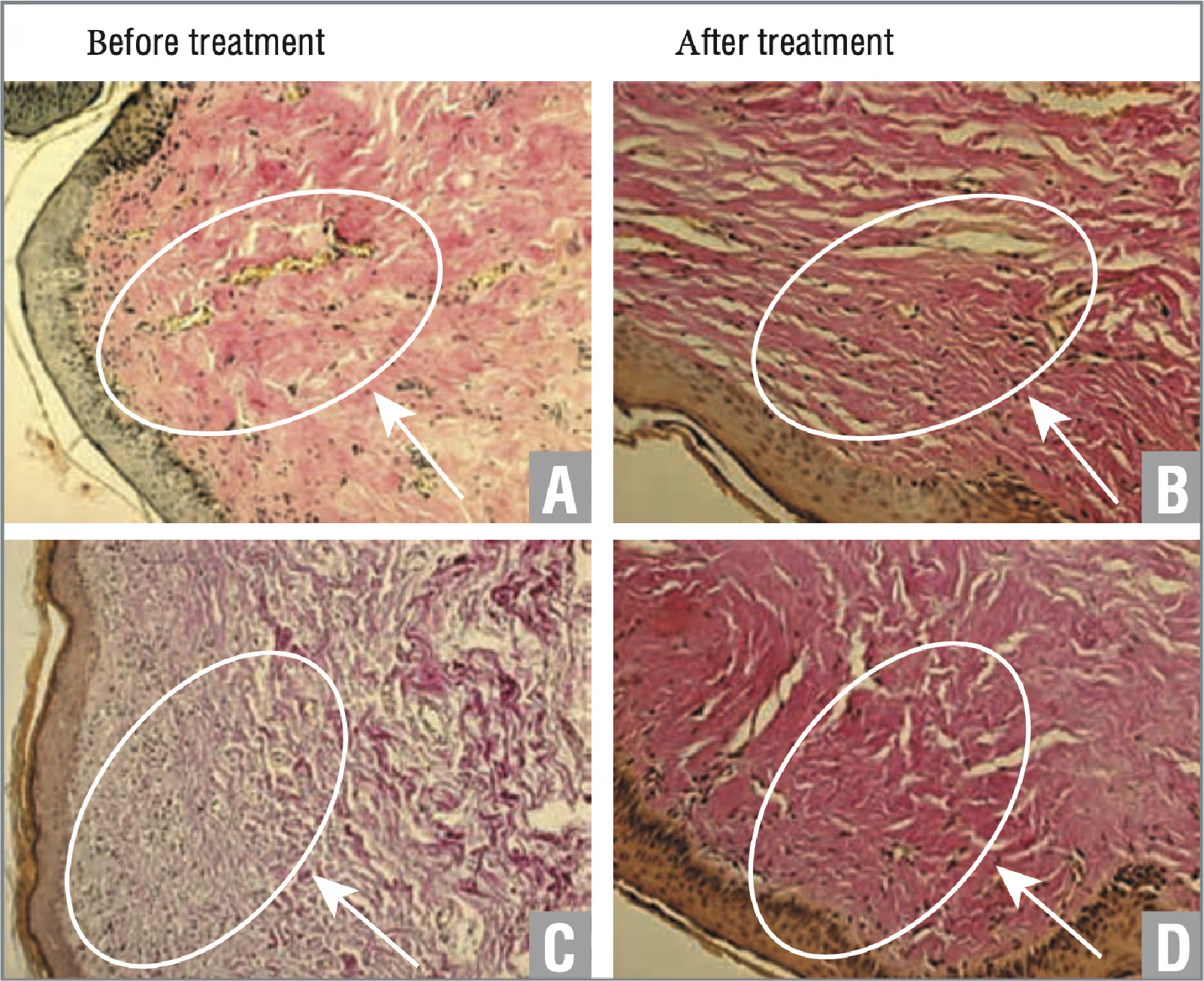
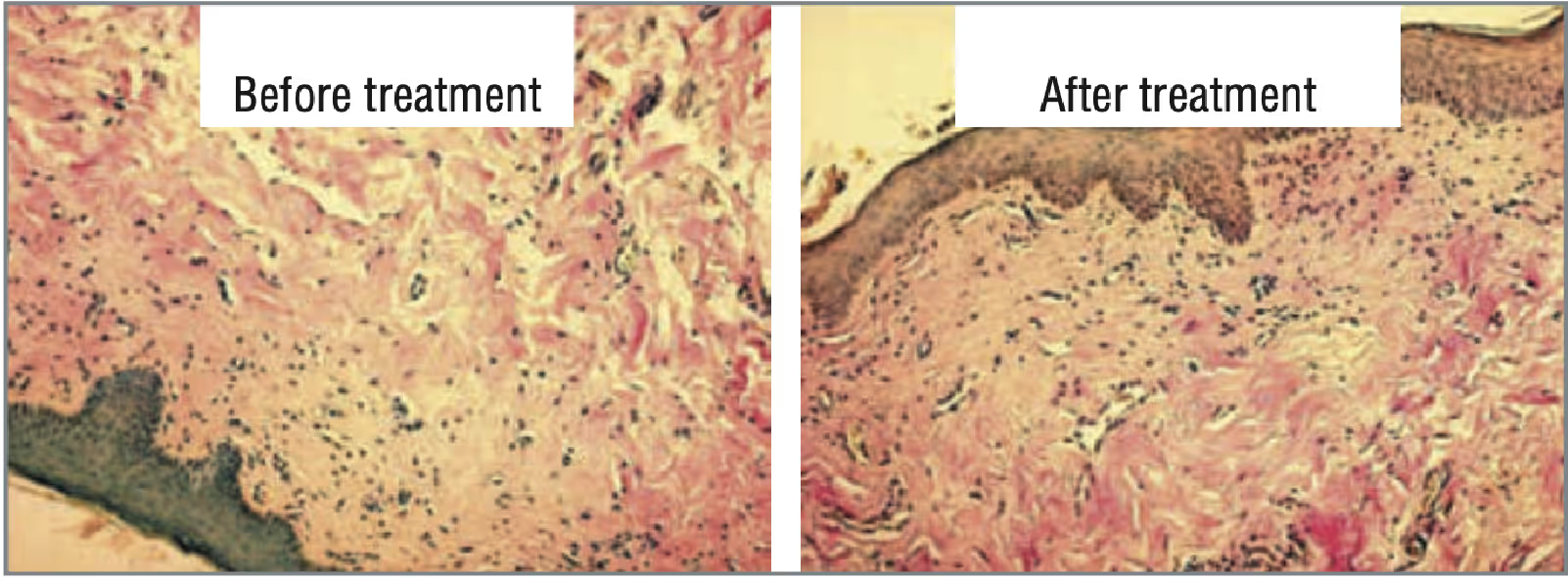
During the exposure to the neodymium laser, no side effects were observed. During the manipulation and during the day, the patients felt a slight feeling of warmth and a moderate burning sensation. Visually, hyperemia was noted on the skin of the external genital organs, which leveled out within one to two hours after the procedure. The results of histological examination before and after the treatment in patients of Groups 1 and 2 are shown in Figures 1 and 2, respectively. According to the results of the study, in patients of Group 1, a more pronounced, bright red staining of the collagen fibers of the stroma was visualized, which indicates a pronounced collagenization of the stroma after treatment (see Fig. 1). According to the results of the study, patients of Group 2 did not reveal significant changes (see Fig. 2).
As for the results of the assessment of the severity of symptoms according to the VAS, the symptoms of the patients of Groups 1 and 2 were moderately severe before the treatment (Fig. 3), which corresponded to 5–7 points.
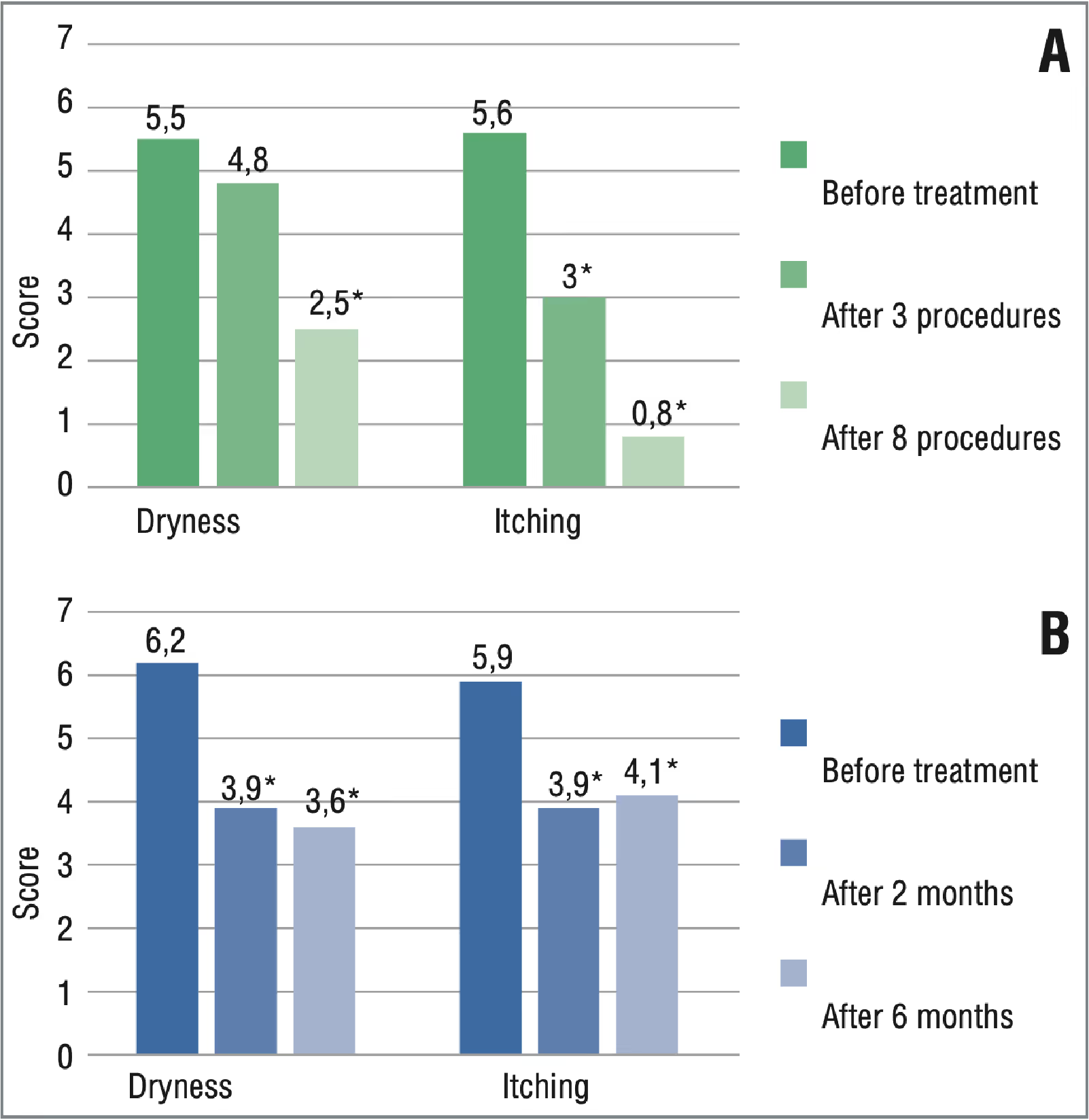
After the courses of treatment, there was a regression of complaints in patients of both groups. According to the results of a two-month follow-up, the patients of Group 2 had lower VAS values compared to the baseline, which indicated the effectiveness of corticosteroids. However, during subsequent follow-ups, the manifestations of symptoms resumed, which indicated a short-term effect of corticosteroid, and further treatment up to 6 months was required (Fig. 4).

In patients of Group 1, during treatment, sexual activity was restored, and libido increased. All patients of Group 1, who were sexually active, noted an improvement in the sensitivity in the intimate area, no dryness and no burning sensation during intercourse. In general, 7 (15%) out of 45 patients were sexually active before treatment. After the end of the course of laser treatment, sexual contact became regular or resumed in 18 (40%) patients (p<0.05). In Group 2, the patients noted an improvement in symptoms during the two-month therapy. However, 9 (60%) patients required maintenance treatment with corticosteroids due to the resumption of symptoms that affected their sex life quality. In a comparative analysis of the obtained results, there is an improvement in performance in the group that under went the laser treatment.
In Fig. 4, the results of the assessment based on the PISQ-12 questionnaire are presented. According to the validated questionnaires (PISQ-12, assessment of the difference in symptoms collected using VAS), 90% of patients showed almost complete regression of complaints associated with itching in the vulvar region after a course of treatment with the neodymium laser. Dryness was significantly reduced in 70% of patients, which significantly reduced discomfort in the vulva.
The visual effect observed in patients of Group 1 (Fig. 5) reflects the changes occurring in the vulva area during the treatment with the neodymium laser. Aerolase Neo ultrashort microsecond pulse stimulates sufficient tissue heating without damaging the epidermis, promoting natural collagen production and improving tissue microcirculation, thanks to which age spots get eliminated, the skin is moisturized, and amore aesthetic appearance is achieved. In patients of Group 2, no visual changes were observed after treatment.
Explicit clinical images below.

Conclusion
The most pronounced and common symptom of LSV is itching of the vulva. According to the validated questionnaires, most patients showed almost complete regression of complaints associated with itching in the vulvar area after a course of treatment with the neodymium laser. Significantly decreased dryness was observed in most patients, which reduced discomfort in the vulva. Unlike patients who received treatment with the neodymium laser, patients who used local corticosteroids noted a resumption of symptoms of itching in the vulvar area, which required them to continue the treatment for up to six months, which shows a short-term effect of corticosteroids.
Based on the study of histological preparations before and after treatment, it can be concluded that neodymium laser treatment promotes pronounced collagenization of the stromain the tissues of the vulva compared to the drug treatment, which indicates the effectiveness of this treatment method for CVD.
Sexually active patients who were treated with the neodymium laser began to notice an improvement in their sex life due to an increase in sensitivity during intercourse, increased libido, and hydration of the skin and mucous membranes, which also increases self-esteem and life quality. Using a neodymium laser is a new safe method for treating degenerative diseases of the vulva with good tolerability and efficacy.
The technology of microsecond laser exposure, unlike other lasers, does not require rehabilitation. Treatment with the Aerolase Neo neodymium laser, due to the combination of wavelength, high pulse energy, and pulse duration (650 ms), is practically painless, does not require contact with the skin, does not damage the skin (non-invasive), and does not cause side effects. Therefore, it is advisable to recommend this treatment to patients with CVD, namely, for treating early-stage vulvar leukoplakia and LSV with moderate manifestations of itching. 8–10 procedures performed within 2–3 weeks are recommended.
References
1. Dobrokhotova Yu. E., Borovkova E.I. Red lesions of the vulva: differentiated approach to diagnosis and treatment. Russian Journal of Woman and Child Health. 2019;2(1):44-48 (in Russ.). DOI: 10.32364/2618-8430-2019-2-1-44-48. 2. Sharapova L.E. To the etiology and pathogenesis of chronic vulvar dystrophic diseases. Russian Bulletin of Obstetrician-Gynecologist. 2010;10(1):29-34 (in Russ.). 3. Latini A., Cota C., Orsini D. et al. Male and femal genital lichen sclerosus. Clinical and functional classification criteria. Postepy Dermatol Alergol. 2018;35(5):447-453. DOI: 10.5114/ada.2018.77236. 4. Ashrafyan L.A., Kharchenko N.N., Babayeva N.A. et al. Lichen sclerosus (kraurosis) as a precancer of the vulva. "Vestnik RTSRR". (Electronic resource.) 5. Semenchak Yu., Snarskaya E. Lichen sclerosus et atrophieus. Vrach. 2018:29(8):26-34 (in Russ.) DOI: 10.29296/25877305-2018-08-07. 6. Zarochentseva N.V. Dzhidzhikhiia L.K. Lichen sclerosus et atrophicus: modern view on the problem. Russian Bulletin of Obstetrician-Gynecologist. 2018;18(6);41-50 (in Russ.) DOI: 10.17116/rosakush20181806141. 7. Virgili A., Minghetti S., Borghi A., Corazza M. Proactive maintenance therapy with a topical corticosteroid for vulvar lichen sclerosus: preliminary results of a randomized study. Br J Dermatol. 2013;168(6):1316–1324. DOI: 10.1111/bjd.12273. 8. Apolikhina I.A., Sokolova A.V., Balashov I.S. et al. Treatment vulvar lichen sclerosus with fractional CO2 -laser: cohort clinical study. Akusherstvo i ginekologiya: novosti, mneniya, obuchenie. 2020;8(2):48– 58 (in Russ.). DOI: 10.24411/2303-9698-2020-12004.