Successful Treatment of Facial Telangiectasias Using a Micropulse 1,064-nm Neodymium-Doped Yttrium Aluminum Garnet Laser
AMY E. ROSE, MD,* AND DAVID J. GOLDBERG, MD†‡
*Ronald O. Perelman Department of Dermatology, New York University School of Medicine, New York, New York;
†Department of Dermatology, Mount Sinai School of Medicine, New York, New York; ‡Skin Laser & Surgery Specialists of New York and New Jersey, New York, New York
Objectives
To evaluate the safety and efficacy of a microsecond 1,064-nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser for the treatment of facial telangiectasias.
Methods
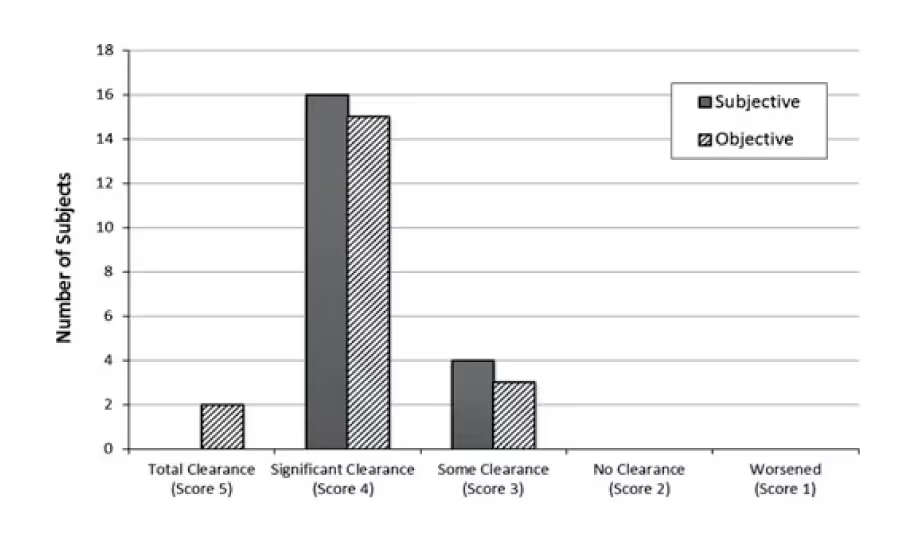
Subjects ages 35–70 with Fitzpatrick skin types I to III and facial telangiectasias underwent two treatments with a micropulse (0.65 ms) 1,064-nm Nd:YAG laser. Treatments were spaced 30 days apart, with a final evaluation 60 days after the second treatment. Evaluation included digital photography and an assessment of the degree of improvement on a scale from 1 to 5 by the subject and a nontreating investigator.
Results
Twenty subjects (18 women, two men) with Fitzpatrick skin type II and III completed the study. The nontreating investigator rated the objective clinical response as total clearance (100% clear) in 10% (n= 2) of subjects, significant clearance ( 50% clear) in 75% (n= 15), and some clearance (0–49% clear) in 15% (n= 3). None of the subjects was rated as having no clearance or worsening. In terms of subjective clearance reported by subjects, 80% (n= 16) reported significant clearance, with the remainder reporting some clearance. No adverse events were reported.
Conclusion
The micropulse 1,064-nm Nd:YAG successfully treated facial telangiectasias with a high degree of patient satisfaction, minimal discomfort, and no adverse events.
This study was funded by a research grant from Aerolase.
Facial telangiectasias are a frequent complaint in patients with fair skin. They are a common sequelae of rosacea and an important component of photoaging. Other causes include medications such as oral contraceptives, overuse of topical steroids, pregnancy, liver disease, radiation dermatitis, and connective tissue disease.1 Once they develop, they seldom resolve spontaneously and cannot be successfully treated with topical or systemic therapies. The most effective treatment for facial telangiectasias is to destroy them using a laser, light source, or electrotherapy. Intravascular oxyhemoglobin selectively absorbs the energy from the laser, which is then released as heat, resulting in destruction of the surrounding vessel.1 Because hemoglobin has a wide absorption spectrum, from 400-nm to 1,100-nm, several wavelengths and light sources can eliminate or reduce the appearance of facial vessels, including the 810-nm diode, 585–595-nm pulsed dye laser (PDL), 532-nm potassium titanyl phosphate (KTP), and intense pulsed light (IPL). Shorter wavelengths such as the 532-nm KTP are effective for smaller vessels but are able to penetrate only 1–2 mm into the skin, limiting their efficacy for deeper telangiectasias, vessels larger than 500 lm, high-flow vessels on the nose, and blue vessels.2,3 The 585- or 595-nm PDL is also effective but has limitations similar to those of the KTP and can cause purpura, especially when used to treat larger reticular veins. In addition, melanin absorbs the KTP and the PDL, which can lead to epidermal damage when used in patients who are tanned or have a Fitzpatrick skin type greater than III.
Longer wavelengths emitted from the 1,064-nm Nd:YAG target the smaller peak of the oxyhemoglobin absorption spectrum in the near-infrared range (700–1,100 nm). The traditional millisecond 1,064-nm Nd:YAG laser has the ability to penetrate deeper (4–6 mm) and to destroy small superficial vessels and deeper, larger vessels.1 Previously used primarily in the treatment of leg veins, they are now used to treat various vascular lesions, including telangiectasias. Because the absorption coefficient of hemoglobin is low at 1,064-nm and because water is a competing chromophore, high fluences must be used to obtain vascular destruction, which increases the potential for collateral damage to the skin.2 The traditional millisecond Nd:YAG laser has been shown to be associated with a significantly higher risk of scarring than the KTP laser for the treatment of vascular lesions such as cherry angiomas.4 A 1,064-nm Nd:YAG laser with a microsecond pulse duration may be able to treat small vessels with less pain and with a better risk profile than the traditional millisecond-pulse-duration Nd:YAG. The purpose of this prospective, single-center, proof-of concept trial was to evaluate the safety and efficacy of a microsecond-pulse 1,064-nm Nd:YAG laser in the treatment of facial telangiectasias.
Methods
Men and women with mild to moderate facial telangiectasias were enrolled from the private practice of the author (DG). Inclusion criteria were ages 35–70, Fitzpatrick skin type I to III, nonsmoker, and willing to use sunscreen for the duration of the study. Subjects who had significant skin disease at test areas, history of poor wound healing, history of keloids, human immunodeficiency virus, hepatitis, immune compromise, pregnancy, lactation, or use of isotretinoin in the past 6 months were excluded. All subjects signed informed consent, and an independent institutional review board approved the study.
Subjects underwent two treatments of facial telangiectasias 30 days apart with a micropulse 1,064-nm Nd:YAG laser (LightPod Neo Aesthetic Laser with MicroPulse-1064 Technology, Aerolase, Tarrytown, NY). Treatment settings were a 2-mm spot size, 0.6-ms pulse duration, and a fluence of 191 J/cm2. Ice packs were applied immediately after treatment. A nontreating investigator assessed clinical improvement of facial telangiectasias by comparing photographs taken 60 days after the second treatment with pretreatment photographs. Degree of improvement was based on a rating scale from 1 to 5 (1= worse, 2= no clearance (0% clear), 3= some clearance (0–49% clear), 4= significant clearance (50% clear), 5= total clearance (100% clear)). Subjects were also asked to report their perceived degree of improvement based on the same scale. The presence and severity of the following side effects was specifically assessed in all subjects: erythema, edema, crusting, bleeding, purpura, blistering, hypopigmentation, hyperpigmentation, and scarring.
Results
Twenty subjects were enrolled, and all completed the study. Ninety percent of subjects were female; 60% were Fitzpatrick skin type II, and 40% were type III. At the final assessment 60 days after the second treatment, the nontreating investigator rated the clinical response as total clearance (score 5) in 10% (n = 2), significant clearance (score 4) in 75% (n = 15), and some clearance (score 3) in 15% (n = 3) (Figure 1). Eighty percent of subjects (n = 16) reported significant clearance (score 4), with the remainder (n = 4) reporting some clearance (score 3) (Figure 1). Pre-and post-treatment photography demonstrated appreciable clearance of facial telangiectasias. (Figures 2 and 3). None of the subjects or the investigator reported a score of no clearance (score 2) or worse (score 1). Subjects reported only minimal discomfort that was mild and transitory. There were no cases of purpura and no other adverse events reported.
Figure 1
Discussion
In our proof-of-concept study, we show that the micropulse 1,064-nm Nd:YAG laser is a safe and efficacious treatment option for facial telangiectasias. Historically, the most commonly used lasers for the treatment of facial telangiectasias have been the 585–595-nm PDL and the 532-nm KTP laser. Although highly effective, shorter wavelengths can cause purpura and epidermal damage, especially when treating larger-caliber vessels. These lasers can also cause permanent sequelae such as hypopigmentation and scarring when used on tanned patients or those with skin of color. Before the current report, there were two main studies that assessed the efficacy of the 1,064-nm Nd:YAG in the treatment of facial vessels, both of which used a millisecond pulse duration. In the first study, from 2002, 17 patients with spider telangiectasias and larger reticular veins were treated with 125–150 J/cm2 and a 25-ms pulse duration and 150 J/cm2 and a 50–100-ms pulse duration, respectively. The authors reported >75% improvement in 97% of the treated sites, with 100% response in all of the periorbital reticular veins treated.5 A few of the older subjects in the study experienced purpura, which the authors attributed to overly aggressive fluences in the range of 125–150 J/cm2 when 100–140 J/cm2 would likely have achieved the same result. It was also noted that the smaller vessels were less responsive than the larger veins even at the shortest pulse width feasible on the millisecond device.5 Thus, it is possible that the microsecond-pulse Nd:YAG used in our study may be better able to target these small vessels that are less responsive to the millisecond Nd:YAG without having to use an excessive, potentially dangerous amount of energy.
Figure 2

Figure 3

In a second study conducted by our group in 2003, 15 subjects with facial telangiectasias on the cheeks or nose had one side of the face treated with a 1,064-nm Nd:YAG laser at fluences of 120–170 J/cm2 and a pulse duration of 5–40 ms for two treatment sessions 30 days apart.6 On an improvement scale of none, mild, moderate, or significant, 80% of subjects had moderate or significant improvement 3 months after the first treatment, although two experienced blistering at the treatment site, even with vigilant epidermal cooling. In the current study, the microsecond-pulse Nd:YAG yielded a comparable degree of clearance of facial vessels, with 85% of subjects obtaining total or significant clearance after two treatments. In contrast to our previous study of the millisecond Nd:YAG, there was no need for epidermal cooling, and there were no episodes of blistering or purpura using the microsecond device.
With the development of longer wavelengths, longer pulse durations, and dynamic cooling devices, the PDL ultimately emerged as the criterion standard for the treatment of unwanted facial vessels,7 but it is notorious for its potential to create cosmetically unacceptable purpura. Although the long-pulse PDL can eliminate purpura, some investigators have noted inferior results to those achieved with purpuric settings.8 A split-face study comparing subpurpuric multiple pass and stacked-pulse PDL with the high-power pulsed KTP laser for the treatment of facial telangiectasia in 14 subjects showed the KTP to be more effective, obtaining the same degree of clearance (75%) in only two treatment sessions as with three sessions for the PDL.7 In the 9% of subjects with purpura, all episodes occurred on the PDL-treated side. Similarly, a study of the 980-nm long-pulse diode laser demonstrated significant clearing of facial telangiectasias that required three sessions.3 In our study, we obtained a high degree of clearance and patient satisfaction in only two sessions and without any purpura. Thus, the micropulse Nd:YAG may reduce the risk of epidermal damage and purpura without compromising efficacy. Previous studies have demonstrated that the 1,064-nm Nd:YAG laser causes more-uniform vessel heating than shorter wavelengths such as 532-nm, which may explain the lack of purpura even at microsecond pulse durations.9
Another notable finding from the split-face KTP/PDL study was that several subjects requested to be retreated on the PDL side with the KTP laser after noting clearance of lentigines on the KTP-treated side. Although the micropulse 1,064-nm Nd:YAG does not target pigment, it has been shown to be effective for laser hair removal, making it a versatile device in a cosmetic practice.10 A distinct advantage of the shorter pulse duration is a better safety profile in patients with skin of color. The shorter wave-length lasers, even when used with intense cooling, are risky in patients who are tanned or have skin of color. The 1,064-nm Nd:YAG bypasses the epidermis due to poor absorption of the wavelength by melanin but in turn runs the risk of damage to the dermis and epidermis because of the high fluences and overheating of all layers of the skin. When using the traditional Nd:YAG laser, which has pulse durations in the millisecond range, a longer pulse duration is safer because the slower rate of heating allows for the dissipation of heat and cooling of the epidermis. The microsecond pulse duration, however, is shorter than the thermal relaxation time (TRT) of both the target (the vessel) and the surrounding skin cells, which have a TRT in the millisecond range (0.8 milliseconds). Thus, the target is heated faster than the rate at which the surrounding skin conducts the heat, minimizing damage to surrounding skin and reducing the risk of pigmentary alteration. Additionally, the pulses travel through the epidermis 30–50 times as fast as the millisecond lasers, which avoids overheating of the epidermis and in turn reduces pain and negates the need for epidermal cooling. Eliminating the need for cryogen cooling further reduces the risk of hypopigmentation, although even faster pulse durations of nano—or pico—seconds can be associated with hypopigmentation when delivered with higher energies. We used a fluence of 191 J/cm2 in the current study, but our subjects were limited to those with Fitzpatrick skin types II and III. When using the 0.65-microsecond Nd:YAG laser in darker skin types, lower energy would be required to prevent pigmentary alteration.
The lack of an untreated control group and the presence of only a single evaluator of the clinical photos somewhat limit the conclusions of this study. In addition, the study was not designed to compare the efficacy of the micropulse Nd:YAG with other wavelengths. Thus, we cannot compare the efficacy of this device with the PDL, KTP, or IPL.
Conclusion
The micropulse 1,064-nm Nd:YAG resulted in significant clearance of facial telangiectasias in the majority of subjects treated, with no adverse events. It offers an additional, efficacious option in the treatment of facial telangiectasias in light skin patients and should potentially be considered as a first-line treatment in patients with darker skin types. Larger comparative studies are needed to compare the safety, efficacy, and efficiency of the micropulse-1,064-nm Nd:YAG with that of the more commonly used shorter wavelengths.
References
- Hare McCoppin HH, Goldberg DJ. Laser treatment of facial telangiectases: an update. Dermatol Surg 2010;36:1221–30.
- Lee JH, Na SY, Choi M, et al. Long-pulsed Nd: YAG laser: does it give clinical benefit on the treatment of resistant telangiectasia? J Eur Acad Dermatol Venereol 2011;26:1280–4.
- Dudelzak J, Hussain M, Goldberg DJ. Vascular-specific laser wavelength for the treatment of facial telangiectasias. J Drugs Dermatol 2009;8:227–9.
- Pancar GS, Aydin F, Senturk N, et al. Comparison of the 532-nm KTP and 1064-nm Nd:YAG lasers for the treatment of cherry angiomas. J Cosmet Laser Ther 2011;13:138–41.
- Eremia S, Li CY. Treatment of face veins with a cryogen spray variable pulse width 1064 nm Nd:YAG Laser: a prospective study of 17 patients. Dermatol Surg 2002;28:244–7.
- Sarradet DM, Hussain M, Goldberg DJ. Millisecond 1064-nm neodymium:YAG laser treatment of facial telangiectases. Dermatol Surg 2003;29:56–8.
- Uebelhoer NS, Bogle MA, Stewart B, et al. A split-face comparison study of pulsed 532-nm KTP laser and 595-nm pulsed dye laser in the treatment of facial telangiectasias and diffuse telangiectatic facial erythema. Dermatol Surg 2007;33:441–8.
- Srinivas CR, Kumaresan M. Lasers for vascular lesions: standard guidelines of care. Indian J Dermatol Venereol Leprol 2011;77:349–68.
- Black JF, Wade N, Barton JK. Mechanistic comparison of blood undergoing laser photocoagulation at 532 and 1,064 nm. Lasers Surg Med 2005;36:155–65.
- Khatri KA, Lee RA, Goldberg LJ, et al. Efficacy and safety of a 0.65 millisecond pulsed portable ND:YAG laser for hair removal. J Cosmet Laser Ther 2009;11:19–24.